A weighty crisis
developmental stages like the gestational stage, the age
group of five to seven years and the adolescence.3 Obesity per se is not a serious health problem, but it is a prime
precursor of many non-communicable diseases (NCDs) like diabetes, hypertension,
cardiovascular diseases (CVDs), gall bladder ailments, cancer, psycho-social problems,
breathlessness, sleep disorders, asthma, arthritis, weak bones and reproductive hormone
abnormalities.
Redefining obesity |
For an early intervention and
right medical treatment, obesity criteria for the Asians need to be redefined
Although research points to the fact that obesity is directly related to diabetes,
interestingly, diabetic cases were reported more in thin people than in people with high
fat content in the body. “Hence, measuring the fat content or body mass index (BMI)
is what really counts in defining obesity”, says Anoop Misra, professor, department
of medicine, All India Institute of Medical Sciences, New Delhi. Asians, in particular,
have a higher propensity for diabetes and heart attacks, as they have higher body fat at
lower BMI. Based on this fact, World Health Organization (WHO) suggested a lower limit for
waist circumference, since Asians with lower waist circumference have been found to have
high BMI. But instead of giving separate obesity criteria for Asians and Caucasians, it
suggested putting lower BMI as a public action health point: between 23 and 27.5
kilo-grammes per square metre (kg/m 2) as overweight and greater than 27.5 kg/m 2 as
obese. But Misra insists that WHO should have separate criteria for Asian population. He
says, “Fifteen per cent of India’s diagnosed population doesn’t get medical
advice and doesn’t even know whether they are obese or overweight. With the new
definition of the criteria to measure obesity, 15 per cent more of Indians will fall under
the gamut of obesity or being overweight.” |
| Source: Sarita Bahl
2004, Wanted an Asian measure of obesity, in Down To Earth,Vol 8, No 8, pp 44-45. |
Governments of several develop-ing countries like India
claim that obesity and NCDs aren’t a problem. But the fact is NCDs are increasing in
these countries at a rapid pace (see
Table: Prime cause of mortality). Even statistics corroborate this. Of the
16.6 million people who died of CVDs in 2001, around 80 per cent were from low and
middle-income countries. It is being feared that by 2010, CVDs would be the leading cause
of death in developing countries. India, China, Indonesia, Pakistan and Brazil are among
the top 10 countries affected by diabetes. About 19.4 million Indians were reported to be
suffering from diabetes in 1995 and this number rose to 31.5 million by 2000. 4 In India, comprehensive programmes for preventing NCDs are either
non-existent or functioning at a very low level. Although many pilot studies have been
initiated, these have not impacted the policy and programme development in any way.
“Programmes for the prevention and control of NCDs need to adopt a ‘life
span’ approach that, in turn, should attempt to reduce risk at any stage of life
through appropriate public health interventions,” says K Srinath Reddy, professor,
department of cardiology, All India Institute of Medical Sciences (AIIMS), Delhi.5
Who is responsible?
“Market forces control the kind of food we eat, which is not good,” says Reddy.
The diversification of soft drink companies into salted food like chips is not by chance.
“This is a way of increasing sales of soft drinks, as salt and oils produce
thirst”, he says. Even fast food chains serving Western food such as burgers and
pizzas are growing by leaps and bounds. Also, unhealthy food tastes good while healthy
food does not. Richard Mattes, professor of food and nutrition at University of Purdue,
USA, has proved that humans can taste fat like they can taste sugar and salt.6 This is in contrast to the general belief of nutritionists and
other scientists that fat only provides texture to food, and that pure fat in itself
doesn’t have any taste.7
How are fast food giants
targeting India?
A Confederation of Indian Food Trade and Industry (CIFTI) document shows the growth in the
major industries, which reflects a shift in the eating habits of Indians (see Graph: Changing food
habits). With the implementation of the World Trade Organization rules, India had to
open itself to foreign investment and multinational companies like Coke and Pepsi, which
entered the market and, being established brand names, managed to get a favourable
response. Currently, some of their popular and best-selling items in the Indian market are
breads, biscuits, chocolates, soft drinks and instant noodles. Their marketing gimmicks
including selling the stuff at a lower price or giving free gifts with the products, have
given a considerable fillip to the sales of their products (see Box: Hooked Fast).
What is happening in Asia
Asian countries are marked by the increasing number of overweight and obese. South Asians
have at least three to five per cent higher body fat when compared to Caucasians.8
Prime cause of mortality |
| Number of deaths due to communicable
and non-communicable diseases |
| Country
|
Communicable diseases |
Non-commu-
nicable diseases |
| Africa |
7,779 |
2,252 |
| USA |
875 |
4,543 |
| Eastern Mediterranean |
1,746 |
2,030 |
| Europe |
567 |
8,112 |
| Southeast Asia |
5,730 |
7,423 |
| West Pacific |
1,701 |
9,000 |
Note: All
figures multiplied by 1,000.
Source: Robert Beaglehole 2003, WHO. Presentation based on World Health
Report 2003. |
China
The current obesity rate in China is below five per cent, but it should be noted that the
obesity prevalence rate is 20 per cent in some of its cities.9 In 1997, 15.4 per cent of the Chinese population was overweight. 10 The incidence of obesity-related NCDs has increased over the past
few years. Experts blame it on mechanisation of the country as well as government
policies. According to Tsung O Cheng, professor of medicine, George Washington University,
Washington, DC, “Any foreigner who visited China in the 1970s and 1980s could not
help being impressed by the phenomenal number of bicycle riders. Bicycling was not only a
necessary means of trans-portation but also a very healthy form of exercise. With a rapid
increase in automobiles, people no longer derive the health benefit of cycling.” 11 He also opines
that the single child policy in China is also to be largely blamed for the huge rise in
obesity.12 A single child in the family generally has two doting parents,
four grandparents and eight great grandparents who express their love by pampering and
overfeeding him/her. Thus, this overfed child grows into an obese adult, who is at the
risk of contracting various NCDs in the later stages of life.
India
India is also faced with a similar kind of obesity and NCD epidemic, but the reasons here
are slightly different. The unique body composition and metabolism of Indians and Asians
makes them more prone to high deposition of fats and its consequences.13 In 1997, seven to nine per cent of the Indian urbanites were
reported to be obese. In the capital city of Delhi itself, nearly a third of the men and
more than half of the women belonging to what could be termed as the ‘upper middle
class’ are currently overweight.14 Indians belonging to the middle class are adding inches to their fat layers,
which can cut short their lives by 20-30 years. A major share of the problem is in cities
since it is the urban children who are lured by the advertisements selling junk food. Even
schools are endorsing these junk food items by selling these in their canteens (see Box: Slowfood it). “Nearly 15 per
cent of children in Bangalore are obese”, says Kamini Rao, medical director,
Adolescence Clinic, Bangalore, who conducted a study on 1,000 children in the age group
11-18 years. She points out that nearly 80 per cent of these kids belong to the upper
socio-eco-nomic strata. Irregular food habits coupled with insufficient playing grounds
was also cited as a main reason behind the growing obesity epidemic.15 Umesh Kapil, a leading nutritionist in AIIMS, in a Delhi survey
of well-to-do schools found that about 27 per cent of school children were overweight and
seven per cent obese.16 He
believes that the main factor responsible for the rising prevalence of this disease is the
lack of physical exercise.
Changing food habits |
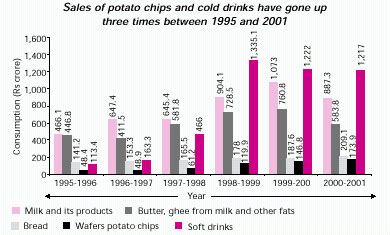 |
| Parna Dasgupta 2004, director,
Confederation of Indian Food Trade and Industry (CIFTI), New Delhi, |
Health impacts of obesity
Obesity substantially increases the risk of morbidity from hypertension; type 2 diabetes;
coronary heart disease; stroke; gall bladder disease; osteoarthritis; sleep disorders and
res-piratory problems; and endometrial, breast, prostate, and colon cancers. Higher body
weight is also associated with an increase in all-cause mortality.
Diabetes
Presently, almost 12 per cent of the Indian urban adults (approximately 280 million) above
20 years suffer from diabetes. The first reliable data on the prevalence of diabetes in
India came from the Indian Council of Medical Research, New Delhi, in the 1970s.
Currently, the country bears 17 per cent of the global burden of diabetes.17 Anoop Misra, professor, AIIMS, studied the relationship between
obesity and diabetes among 2,000 school and college students of New Delhi. His study
revealed that almost one-fourth of the obese children were insulin resistant — a
stage that can lead to diabetes. “Nearly 43 per cent had sub-clinical inflammation
that is a future indicator of diabetes and heart disease,” he says.18
C Yagnik, researcher at the King Edward Memorial Hospital and Research Centre, Pune,
investigated the aspects of body size of rural and urban Indians in relation to their
meta-bolic and endocrine characteristics.19 It is being estimated that by 2015, diabetic population will be
the highest in India, with maximum patients being under the age of 40 years.20 Indians tend to be diabetic at a very young age of 45, after
which the life expectancy is, on an average, eight years only.21 The early onset of diabetes is mainly due to the changing food
habits. A couple of years ago, people in the age group of 20-35 years used to suffer from
diabetes. But now, children aged anywhere between three months and 17 years are also
developing diabetes, which is a cause for great concern.22

